Pediatricians’ obesity guidelines rest on shaky evidence about eating disorder risks
By Kate Raphael. This story was originally published by STAT News on September 16, 2024.

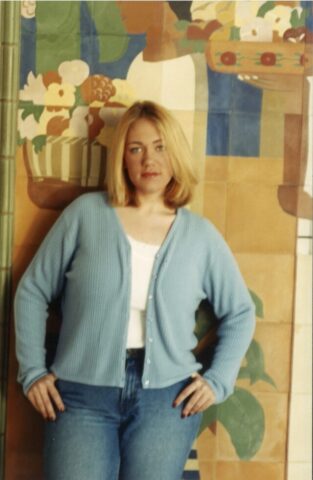
Joslyn Smith said she worries new obesity guidelines will inadvertently cause some young people to develop eating disorders. “I have no doubt that people are going to die because of this,” she said. / Heather Ainsworth for STAT
Joslyn Smith said she worries new obesity guidelines will inadvertently cause some young people to develop eating disorders. “I have no doubt that people are going to die because of this,” she said. / Heather Ainsworth for STAT
To address soaring rates of childhood obesity, the American Academy of Pediatrics last year endorsed tactics it once considered risky.
“Watchful waiting” had been standard practice, in part from concern that a doctor’s focus on weight could inadvertently plant the seed for stigma or eating disorders like anorexia and bulimia.
The influential academy now said pediatricians should pursue “early treatment at the highest level of intensity appropriate for and available to the child.” Some teenagers should undergo bariatric surgery. Others should inject the obesity drug Wegovy. Some children as young as 2 should undergo intensive behavioral treatment.
The AAP cited three academic papers to support its conclusion that aggressive obesity treatments would not fuel disordered eating, saying the literature clearly “refutes this relationship.” But in interviews with STAT and the Investigative Reporting Program at UC Berkeley’s Graduate School of Journalism, authors of each paper said the pediatric group misconstrued or misused their work. In particular, the authors took aim at the AAP’s claim that eating disorders would be reduced for up to six years after obesity treatment.
The issue is pivotal because pediatricians are also scrambling to contain skyrocketing rates of eating disorders in young people. Eating disorders, which often take years to recover from and can be fatal, now rival asthma as the second most common chronic condition in U.S. children — behind obesity.
One of the three studies cited by the AAP was conducted by Australian scientists, including Megan Gow, a researcher at the University of Sydney, Australia. But Gow said the AAP had “cited the wrong paper.” She thought the academy intended to cite another paper of hers, but that one also lacked any assurance that obesity treatment would reduce eating disorders long-term.
An author of the second paper, University of Buffalo professor Katherine Balantekin, said she was only familiar with limited data indicating that the risk of eating disorders may be reduced in the short term. “All of our data that I’m familiar with don’t go out to six years, so I’m trying to think of what they would have used,” she said.
Heather Forkey, a pediatrics professor at the University of Massachusetts, authored the third paper, a report on treating patients with trauma. She said inclusion of her work must have been a “typo” because it didn’t discuss eating disorders. “I am not sure that I know why we were quoted,” she said.
The guidelines’ lead author, Sarah Hampl, director of the Center for Children’s Healthy Lifestyles and Nutrition at Children’s Mercy in Kansas City, Mo., has defended the new recommendations against criticisms by eating disorder experts. Hampl acknowledged that evidence scrutinizing the long-term relationship between obesity treatment and eating disorders was thin — calling it “a gap in the literature.” She added, “A lot of studies did not report eating disorders or disordered eating outcomes.”
But she said the AAP remained confident in the recommendations’ safety because, in addition to the research, the guidelines “underwent extensive review by numerous committees and councils within the AAP,” including experts on eating disorders and obesity.
The AAP has also formed a work group of eating disorder experts to contextualize the guidelines with education to help doctors and parents guard against eating disorders while still adhering to the aggressive approach to obesity.
One work group participant, Christine Peat, a nationally recognized eating disorder expert at the University of North Carolina, called the work productive. She recognizes the challenge of revising published guidelines, yet she said, “The eating disorder provider in me says, ‘Yes, absolutely, they should walk back from the guidelines.’” Such worries, she said, remain “fairly uniform” among eating disorder specialists.
“There is a real risk that some of these kids may be inadvertently sort of set up for an eating disorder,” Peat said.
Following interviews about the errors uncovered by the reporting for this article, the AAP updated its recommendations, replacing one of the three cited papers with a new one.
The new paper, which analyzed the long-term effects of obesity treatment, included just two studies that followed children for at least four years. Both were conducted decades ago in Belgium and attempted to ascertain whether pediatric obesity treatment can trigger eating disorders. But the results were mixed. The studies had small sample sizes, lost track of half the patients or more and had no control groups to determine whether the changes in eating were related to the obesity treatment the children underwent.
One of the lead researchers, Lien Goossens, said her findings “cannot really be generalized to all overweight youth.”
Moreover, Goossens’ study was conducted before most doctors understood that an especially dangerous eating disorder, anorexia, can develop in larger-bodied children as well as those who appear underweight.
Joslyn Smith, a 45-year-old resident of Ithaca, New York, recalls developing anorexia in her adolescence, shortly after a doctor instructed her to lose weight. The AAP’s new obesity guidelines alarm her. “I have no doubt that people are going to die because of this,” she said.
No risk-free solutions
The 2023 guidelines were the first time in 15 years the AAP overhauled its recommendations on childhood obesity, as it noted a major shift in the size of American youth. One out of five children in the United States is classified as having obesity today — quadruple the rate in the 1970s.
This coincides with a rise in children with conditions correlated with obesity including hypertension, diabetes and fatty liver disease. Before the 1990s, type 2 diabetes was rare in children. The Centers for Disease Control and Prevention estimated that 5,000 children and adolescents are now diagnosed with it annually. Fatty liver disease, once virtually undetected in children, now afflicts approximately 5 percent to 10 percent of children.

Smith on her fourth birthday.
Courtesy Joslyn Smith
Given these risks, some experts thought the issue of eating disorders was delaying necessary action. “I’m not going to stop the war on obesity since I worry I might trigger some increase in eating disorders,” said Arthur Caplan, a bioethicist at New York University who believes the known risks of obesity outweigh the potential risks of eating disorders.
Smith on her fourth birthday.
Courtesy Joslyn Smith
When the AAP’s overhaul emerged, Gitanjali Srivastava, an obesity specialist at Vanderbilt University, said it was “very long overdue.” She said the guidelines “do not promote eating disorders, but rather they encourage us providers to really properly assess and evaluate patients that are presenting for disordered eating.”
The Food and Drug Administration helped pave the way for the AAP’s aggressive approach by approving Wegovy in 2022 to treat pediatric obesity, based on a small clinical trial showing that most adolescents taking the drug lost at least 5 percent of their body weight after 68 weeks. The trial was funded by Novo Nordisk, Wegovy’s manufacturer.
Intensive behavioral counseling was also buttressed by the recent endorsement from a powerful federal advisory board, the U.S. Preventive Services Task Force. The task force didn’t recommend weight loss drugs for children and said the evidence to support their use was “inadequate.” Most studies lasted two months or less and did not examine long-term effects. (A new trial found that children ages 6 to 12 taking a GLP-1 experienced modest body mass index reduction. Yet some experts raised concerns about the dearth of long-term data, especially for growing bodies.)
Many others have called for more action to guard against eating disorders, which are especially prevalent and often unrecognized among children and young adults with obesity.
Leslie Sim, a psychologist specializing in eating disorders at Mayo Clinic, said some of her larger-bodied anorexia patients said their eating disorders began when doctors told them “their weight has tracked too high.”
Sim said patients can interpret this as, “The doctor told me that I’m fat,” or “I’m doing something wrong.” Even when they received nuanced messaging about healthy habits, emphasis on weight can lead children to resort to starvation, Sim said.
Cheri Levinson, director of University of Louisville’s eating disorder lab, said “many of our kids and adolescent patients have come to us after developing an eating disorder because of an appointment with a pediatrician.”
The AAP knows that any conversation with kids about weight is risky.
In a 2016 publication, the organization said: “At first, weight loss is praised and reinforced” but extended attention to weight “can lead to social isolation, irritability, difficulty concentrating, profound fear of gaining the lost weight back, and body image distortion.”
When the new obesity guidelines emerged in January 2023, the AAP said that any risk of doctors’ sparking eating disorders can be mitigated through screening. However, interviews with directors of obesity treatment centers — including those cited by the AAP as national models — showed that some do not screen for eating disorders and have little training to handle risks. “There’s not a specific training or tool within this program,” said Kate Heelan, creator of Building Healthy Families, a weight management program in Nebraska listed on the AAP’s website.
Topic 1 for 14,000 conference goers
The national conversation around children’s weight and health tends to focus on obesity rather than eating disorders. Federal funding reflects this imbalance: in 2023, the National Institutes of Health allocated nearly $1.2 billion to obesity and only $55 million to eating disorders.
At the AAP’s national conference last October, attention to the two issues was also lopsided. The new obesity guidelines drew much attention from the more than 14,000 attendees who descended on a convention center in Washington, D.C.
Pediatricians crowded into a room for a full-day workshop on how to use GLP-1s, a class of weight loss drugs including Wegovy. The AAP recommends that physicians discuss the injectables, or alternatives, with all children 12 and older identified as having obesity.
One speaker called GLP-1 drugs “transformational, akin to penicillin.”
Some pediatricians attending the conference said that for decades, treating obesity was hopeless and thought the new approach could be a gamechanger.
Throughout the convention, signs identified the AAP’s major donors, including Novo Nordisk. The founding sponsor of the AAP’s initiative on childhood weight is Nestlé, currently designing a line of food to be used with GLP-1s.
In a written statement after the event, the AAP said that neither company inappropriately influenced the obesity guidelines nor the conference content.
Many speakers focused on obesity and presented the guidelines with enthusiasm, yet dangers of the medications still emerged. GLP-1s can cause rapid weight loss, often 10 percent to 20 percent of body weight. Some presenters noted that this makes it nearly impossible to differentiate medication-driven weight loss from an eating disorder. If doctors aren’t looking for eating disorders, they won’t find them, the panelists said.
Some weight loss drugs can disguise eating disorder symptoms, the presenters said. For instance, one drug combination the AAP recommends, phentermine and topiramate, can cause hypertension, masking a low heart rate and blood pressure, signs of a possible eating disorder.
Bariatric surgery, recommended by the AAP for children 13 and above with severe obesity, also gave some pediatricians pause. A 2019 literature review found that a notable share of candidates for bariatric surgery had binge eating disorder. Recovery from the procedure requires constant attention to diet, which can exacerbate eating disorders.
The lifestyle treatment the AAP recommends for high-weight children 2 and up also raised concerns. In some programs, children step on the scale weekly, complete detailed food logs, and follow the “traffic light diet,” which categories food into “always,” “sometimes” and “rarely” groups, behaviors that some research links to eating disorders. Some programs monitor children’s activity with step trackers and reward them with raffle tickets when they avoid gaining weight, a focus on size and exercise that some clinicians fear will drive eating disorders.
But these worries were easy to overlook: Twenty-three presenters focused on obesity; four spoke on eating disorders.
Cynthia Bulik, a University of North Carolina professor of eating disorders who did not attend the conference, said professionals combating obesity and eating disorders are siloed.
“The biggest problem is that these two fields don’t communicate,” Bulik said. “I think we almost live in separate worlds.”
Less visible anorexia, still dangerous
The studies that best support the AAP’s claim that obesity treatment reduces eating disorders occurred two decades ago in Belgium. They analyzed very different treatment approaches from those the AAP recommends today.
Lien Goossens, one of the Belgian researchers, studied an inpatient obesity clinic, Zeepreventorium, on the nation’s coast. Apart from weekends at home, the children lived for 10 months at the treatment center and received near-constant support during meals, exercise and group therapy, a much higher level of care than the outpatient programs the AAP recommends.
A second Belgian study followed an outpatient cohort of 136 children. In interviews, its authors expressed guarded optimism about the behavioral treatments they studied but said the U.S. is implementing a different approach with less psychological support.
When the researchers conducted their work, many assumed larger-bodied people couldn’t starve themselves. “Anorexia nervosa is not something we would expect to find there, of course,” Goossens said.
It was only in 2013, well after the Belgian work, that the Diagnostic and Statistical Manual of Mental Health Disorders recognized “atypical anorexia” as an eating disorder. Patients with the condition have all the symptoms of typical anorexia except that they are at a weight considered normal or high. Goossens added that, if conducting a study today, researchers should look for other treatment effects, such as depression, low self-esteem and all eating disorders, including atypical anorexia.
Smith in college: At times she ate so little a clinician found she was severely malnourished. She credits an eating disorder treatment center with saving her life.
Courtesy Joslyn Smith
Smith in college: At times she ate so little a clinician found she was severely malnourished. She credits an eating disorder treatment center with saving her life.
Courtesy Joslyn Smith
These patients often obsess over caloric restriction and strive for weight loss. They may fast for long stretches, adhering to strict rules for when certain foods can be consumed. They often suffer heart and gastrointestinal issues, weakened bones, depression and suicidal thoughts. Children may also experience stunted growth, impaired cognition and delayed puberty.
Anorexia, in both the typical and atypical form, is one of the deadliest mental health disorders. One out of 20 die within four years of diagnosis.
Research by University of Denver professor Erin Harrop shows that the atypical disorder happens at least as frequently as the typical form better understood by the general public and physicians. At some treatment centers, atypical anorexia patients represent half those hospitalized for eating disorders.
Still, some data show that high-weight patients wait nearly nine months longer to receive eating disorder diagnoses than patients who are not high-weight. When high-weight patients do seek help, they may face skepticism and disbelief that they are sick. They must confront treatment centers overwhelmed by the crush of cases, which have doubled among adolescents since 2020 and have not returned to baseline.
When Joslyn Smith, of Ithaca, New York, was 15 years old, she saw a doctor for neck pain near her Arkansas hometown. She recalled that the doctor poked at her upper spine and told her it curved into a “buffalo hump,” a pad of fat between the shoulders.
Smith and her mother, Susan Yager, said the doctor prescribed a restrictive meal plan requiring her to vigilantly monitor calories and eliminate sugar. She strictly followed the advice. “Coming from a medical professional, it felt really legitimate and credible,” she said. At a follow-up visit several weeks later, she stepped on the scale, elated that 10 pounds had vanished.
But as quickly as the weight came off, it reappeared, plus several pounds. The cycle continued for years in a pattern that research shows is common.
In college Smith reached her heaviest, close to 300 pounds. She doubled down on her doctor’s approach to weight loss, eating small portions or nothing at all. She purged, over-exercised and ate laxatives, dropping over a third of her weight in a year. Her doctor’s growth chart still said she was overweight, though she was severely malnourished, according to one of her clinicians, Carolyn Chaffee.
Smith passed out on campus multiple times and developed an irregular heartbeat and a dangerously slow pulse. Her potassium levels sank so low that she risked cardiac arrest. Still, she thought she was following her doctor’s advice, his words in a loop in her brain.
At age 22, Smith visited her mom in Arizona. For days, she barely ate and swallowed laxatives. One Sunday at the end of the trip, severely depressed, she attempted suicide.
An eating disorder treatment center saved her life, and in 2002, Smith began talking publicly about her experience. For years, people told her she was an anomaly. “You can’t weigh 250 pounds and have anorexia,” she remembers hearing. Smith has worked for decades to show that she is not an exception. She has taken on policy roles for the American Psychological Association and National Eating Disorders Association to expand diagnosis and recognition of all eating disorders in high-weight people.
Now, 30 years after that doctor’s appointment, Smith worries that the guidelines put millions of children at risk of repeating her experience.
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.


